Share on
Diagnosing your child
Diagnosing any child is especially challenging and depends on the type of amblyopia. Since a child is usually not able to tell us what they are experiencing, as a parent it’s important to be on a constant lookout for signs pointing to visual problems and consult with a primary healthcare provider for monthly eye screenings.
Common types of refractive error
Refractive amblyopia is usually less severe than strabismic amblyopia and is commonly missed by primary care physicians because of its less dramatic appearance and lack of obvious physical manifestation.
A healthcare provider will look for signs of abnormality such as Strabismus, Nystagmus which is an involuntary shaking of the eyes and other structural abnormalities of the eye itself. Some other diagnostic tests during screening might be checking whether a baby blinks to light and is able to fixate on objects. Around the age of 3-5 a doctor will be able to screen a child in more detail with tests often used with adults such as with a child-friendly visual chart.
Along with these behavioral methods, a primary healthcare provider might also use a machine to estimate a child’s refractive error and in some cases even detect Strabismus. An important thing to understand is that a machine will not diagnose amblyopia in a child.
Instead it will pick up risk factors that might put a child in danger for developing amblyopia in the future. In this case, a more detailed examination by an ophthalmologist might be necessary and treatment will depend on a child’s individual diagnosis.
Treating Amblyopia
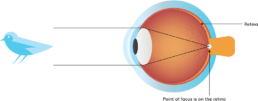
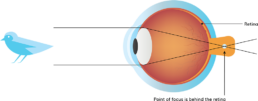
The first step to treating amblyopia is addressing the risk factor causing it. In the case of Deprivation Amblyopia, it’s important to remove cataracts or elevate the drooping eyelid through surgery. If the child is diagnosed with Refractive Amblyopia, they might need to wear glasses to correct for the blurry vision.
Some research shows that treating refractive amblyopia with glasses alone can improve visual acuity in more than 50% of children between the ages 3-7, with the numbers decreasing the older the child is. Things, however, are a little different when it comes to strabismus.
In this case, it’s important to treat strabismus first before attempting surgery because of the better a child’s vision before surgery, the higher the chances of good surgical results.
Most of the existing treatments for Strabismus focus on limiting the visual acuity in the healthy eye by blocking it completely or blurring it to give the brain more time with the amblyopic eye. One of the most commonly prescribed methods is eye patching.
A healthcare provider may ask you to patch a child’s “good” eye. In theory, the brain should stop ignoring the visual inputs from the “lazy eye”. The patch should be applied for a few hours daily, depending on the severity of amblyopia and can also be applied beneath eyeglasses. The main concern with eye patching is that they are often an unpopular treatment. Children might refuse to keep the patch on and try “peaking”, making the treatment ineffective.
In this case, an alternative that is often prescribed is eye drops. With a similar principle as the eye patch, the drops are applied to the healthy eye in order to “blur” it and encourage the brain to accept input from the “bad” eye as well. Although eye drops might be easier to use, they significantly decrease a child’s vision in the healthy eye and might cause confusion.
Studies have also shown that they are only effective for cases of mild amblyopia and can often lead to photosensitivity in the eyes because of dilating effects on the pupil. A similar treatment is placing a transparent Bangerter filter over the lens of the healthy eye in order to blur it.
Surgery and risks
Treating amblyopia is dependent on a child’s compliance to wearing their glasses, eye patch or keep taking the drops. An ophthalmologist might recommend surgery, depending on the type of amblyopia. Eye muscle surgery is a method performed for treating strabismus. This surgery involves moving one or more eye muscles for adjusting the position of the misaligned eye(s). Although a relatively safe and commonly performed surgery, there are risks involved that should be taken into account beforehand.
These include possible reactions caused by anesthetics that might result in permanent vision loss, damage in the retina or nerve or permanent double vision. In the case of an under or overcorrection, the eyes might turn another way and a second operation might be needed to restore a normal eye alignment.
Reference:
https://www.surgeryencyclopedia.com/Ce-Fi/Eye-Muscle-Surgery.html#ixzz6KFEf6XbT
Refractive surgery is sometimes performed in trying to correct for Refractive Amblyopia. This involves reshaping the cornea or planting a lens inside the eye to improve the eye’s focusing ability. This surgery reduces the cornea’s curvature for nearsightedness, attempt to achieve a steeper cornea for farsightedness and reshape an irregular cornea in the case of astigmatism.
This method is not universally accepted and also bears some risks since a child’s eyes are still growing and their refractive error is constantly changing. Considering the significant risk of surgery, it’s good to consider alternative options before making a decision.
Dichoptic Therapy
A recently popular alternative to methods like eye patching and surgery is dichoptic therapy. This is a method of treating Amblyopia where images are presented to both eyes at the same time but separately. This is done by using different contrasting images.
The amblyopic eye receives higher contrast images and the healthy eye register lower contrast images. The patient has to combine the input with both eyes (binocularly) in order to perform the task which is often something fun such as a video game.
Since each eye selectively gets limited information on the picture in front of them, the brain is forced to use the visual information in both in order to produce a full meaningful picture
bloo vision is an example of such a therapy. By using a tablet and glasses with a special coating, a child can play games that are entertaining and at the same time force the brain to process the varying visual input from each eye. This trains the amblyopic eye and might be easier when it comes to compliance.
Early diagnosis and treatment of amblyopia are crucial for preventing the visual disorder in adulthood. After being informed about the different types of amblyopia and choosing the therapy most suited to a child’s need, treatment should be early and consistent in order to ensure a lifelong good vision for your child.
References:
Holmes JM, Repka MX, Kraker RT, Clarke MP (March 2006). “The treatment of amblyopia”. Strabismus. 14 (1): 37–42. doi:10.1080/09273970500536227.
About vision therapy. College of Optometrists in Vision Development. www.covd.org. (Accessed February 2016.)
What is vision therapy? Optometrists Network. www.visiontherapy.org. (Accessed February 2016.)
Neuroplasticity: Teaching an old brain new tricks. Review of Optometry. January 2009.
Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Archives of Ophthalmology. October 2008.
Practice and perfect: length of training and structural brain changes in experienced typists. NeuroReport. July 2007.
A randomized clinical trial of treatments for convergence insufficiency in children. Archives of Ophthalmology. January 2005.
Williams C, Northstone K, Harrad RA, Sparrow JM, Harvey I (June 2002). “Amblyopia treatment outcomes after screening before or at age 3 years: follow up from randomised trial”
Li T, Qureshi R, Taylor K (2019). “Conventional occlusion versus pharmacologic penalization for amblyopia”